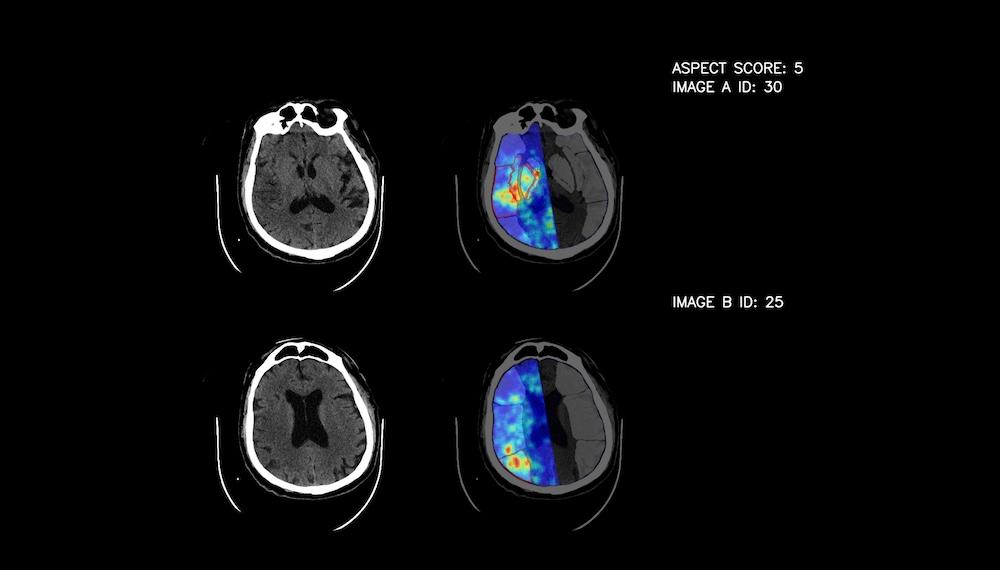
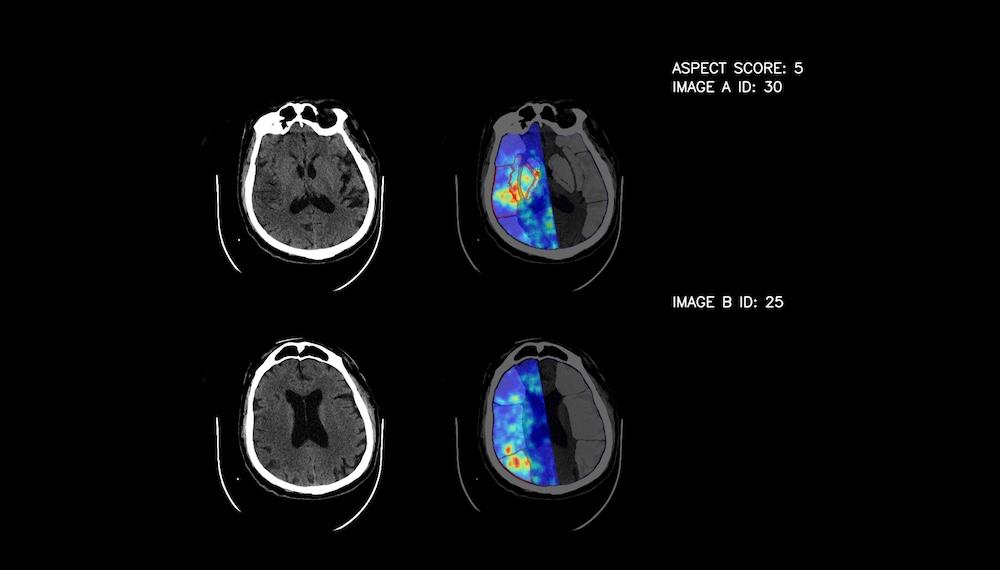
The Latvian artificial intelligence solutions developer "Apply", in collaboration with radiologists Assoc. Prof. Kārlis Kupčs and Dr. Andris Veiss, has created a solution called "Sinapse", which assists the Stroke Unit of Pauls Stradiņš Clinical University Hospital (PSCUH) in detecting ischemic stroke with 93% accuracy. This makes it one of the most effective tools of its kind in the world.
Labs of Latvia previously reported that a year ago, the PSCUH Stroke Unit began using Sinapse, a solution jointly developed by a local tech company and medical professionals. Since then, the tool has analyzed the radiology scans of more than 1,000 patients, flagging potential signs of stroke for physicians.
“The AI assistant has become a real support in the daily work of radiologists, especially considering the diagnostic accuracy improvements of Sinapse. We can review results faster, meaning patients receive help more quickly. In stroke cases, that’s a critical benefit for reducing long-term complications,” says Assoc. Prof. Kārlis Kupčs.
Over the past year, the tool's accuracy has increased by 13 percentage points, now reaching 93% effectiveness. Even in its early stages, doctors already recognized Sinapse as one of the most accurate among international competitors. Other tools previously tested by the hospital had shown only around 60% success rates. After nearly a year of use in the hospital and additional calibration, it has become even more "perceptive." Kupčs says he is surprised that such high precision was achieved with a relatively small data set.
“We’ve completed the pilot project phase, during which, thanks to constant interaction between physicians and our colleagues – the AI developers – we continued training and calibrating the tool to enhance its analytics capabilities. We've increased the stroke detection accuracy by 13 percentage points, now reaching 93%,” explains Līna Briņģe, Head of Production at Apply.
Faster Help for Patients
Ischemic stroke is the second leading cause of death and the third leading cause of disability in the world, including in Latvia. Timely assistance is crucial for patients – ideally within the first two hours. Kupčs previously explained that stroke, caused by the blockage of brain arteries, is treatable today – the key is early hospital intervention. When a stroke occurs, approximately two million neurons die every minute. Although our brain contains billions of such cells, each one is responsible for a specific function.
“In the early hours of an ischemic stroke, changes on CT scans are either not visible or are extremely minimal, making it difficult to recognize them with the naked eye. That requires experienced specialists and a complex symptom analysis,” emphasizes Kupčs.
With Sinapse, evaluating a CT scan takes approximately 15 seconds, which significantly accelerates patient care.
Briņģe has previously emphasized that no tool or device can replace a doctor. However, artificial intelligence can become as sharp-eyed as a doctor, with the main goal being to serve as a supportive assistant.
“Teaching the system to ‘see’ like a healthcare professional is a major challenge. Medical data is highly specific and complex, so during development we work closely with radiologists to ensure the tool’s accuracy,” says Briņģe.
Diagnosing Other Conditions
Discussions are already underway to roll out Sinapse in other medical institutions.
“We hope that Sinapse will also be available in regional hospitals in the future. In those hospitals, radiologists are often consulted remotely – AI could significantly simplify that process,” says Kupčs.
The developers are also training the tool to recognize the next most common brain injury after stroke – hematomas, or internal bleeding, which can result from head trauma or other pathologies.
A hematoma forms when a damaged blood vessel leaks and the blood displaces surrounding tissue instead of being absorbed, forming a cavity. It’s crucial to identify hematomas early and distinguish between their types in order to apply the appropriate treatment. Sinapse is expected to be able to both detect and classify such events in the near future.
“Stroke detection was always intended as the first step in the development of the tool. Now that it can reliably identify stroke, we can begin teaching it to recognize other pathologies. Intracranial hematomas, like strokes, are time-sensitive and require immediate care. That’s why they’ve become our next focus. Later, we plan to train the system to detect brain tumors and various inflammatory conditions as well,” says Kupčs.